Preventive practices
Alimentary prophylaxis
The gut hypothesis
When you see a septic patient crashing in the ICU, a natural question to ask is where the source of infection comes from. The hypothesis that pathogenic organisms mainly originate from being introduced through catheters has been put into question (if this were the case, why are peripheral catheters not a risk factor for sepsis?), and the “gut hypothesis” has become a prevailing theory of the origin of sepsis.
The gut hypothesis claims that hypoperfusion to the gut allows for intermittent ischemia and allows translocation of enteric bacteria into the bloodstream (hence the prevalence of enteric organisms found in sepsis). This eventually leads to a positive feedback loop leading to multiorgan failure1.
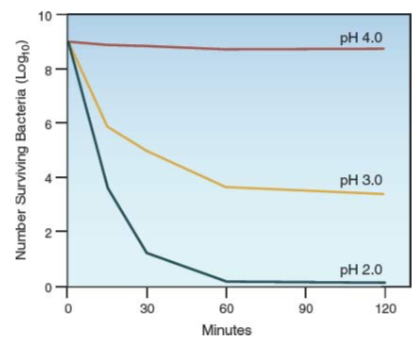
Gastric acid
Gastric acid has a role in creating a sterile environment in the stomach, and has a less important role in nutrient digestion/absorption. This is why people with achlorhydria do not suffer malabsorption2.
Stress ulcers
Almost every patient in the ICU probably has an oozing gastric ulcer3. Although fewer than 5% of patients ultimately go on to develop clinically significant bleeding, prophylaxis should probably be implemented in most or all of these patients.
Gut prophylaxis options
| Medication name | Drug class | Mode | Dosing |
|---|---|---|---|
| Famotidine | H2 blocker | IV | 20mg Q12h |
| Ranitidine | H2 blocker | IV | 50mg Q8h |
| Lansoprazole | PPI | NG | 30mg QD |
| Omeprazole | PPI | NG | 20mg QD |
| Pantoprazole | PPI | IV | 40mg QD |
| Sucralfate | Protectant | NG | 1g Q6H |
H2 blockers
- Dose renally, as overdosing can cause agitation and confusion in those with renal failure
- Very slight increased risk of C. diff infection or aspiration pneumonia
Proton pump inhibitors
- More potent than H2 blockers
- Does not require renal dosing
- Higher risk of infection (GI, pulmonary) compared to H2 blockers
- Can impede clopidogrel antiplatelet activity4!
Sucralfate
Sucralfate doesn’t have an effect on gastric acid secretion. It does, however, bind to the denuded surface of an ulcer and protect it from further damage.
Sucralfate interacts with ciprofloxacin and norfloxacin, so should be spaced if the patient is taking either of these medications. Patients with hypophosphatemia probably should not be on sucralfate.
Enteral feeding
Patients who receive tube feeds probably do not require further prophylactic measures for stress ulcer bleeding. However the data is still sparse on this topic, so maintain a low threshold to start medical stress ulcer prophylaxis.
Venous thromboembolism
We’ll go through some of the risk factors one by one in this section and talk about some salient learning points.
Risk factors
Major surgery
Risk of VTE is highest after orthopedic surgery, particularly involving the knee or hip5. Risk is also high in patients who undergo cancer-related surgery5.
Trauma
Highest risk is in brain and spinal cord injuries, spinal fractures, and fractures of the hip and knees (think prolonged immobility).
Acute medical illness
Risk factors include cancer, mechanical ventilation, sepsis, prolonged immobility.
Prophylaxis
Let’s go over some possible options for thrombophylaxis.
Unfractionated heparin
As the name suggests, this is a heterogeneous mixture of heparin in many molecular weights. Only a third of the mixture has anticoagulant activity! UFH works mainly through inhibition of thrombin (factor IIa) and factor Xa (anti-IIa » anti-Xa activity)6.
Beware: heparin can bind to platelets and trigger an IgG-mediated response in a condition known as heparin-induced thrombocytopenia. In obese patients, heparin needs to be re-dosed, since there is an increased VD of the drug.
Low-molecular-weight heparin
In contrast to UFH, LMWH acts on Xa more than IIa. Compared to UFH, LMWH tends to have a more predictable dose-response curve and is more potent, and can be dosed less frequently. Furthermore, there is a lower risk of HIT (heparin-induced thrombocytopenia) compared to UFH. However, it is cleared by the kidneys and therefore needs to be renally dosed.
Enoxaparin vs. dalteparin
These are the two types of LMWH that are most widely used. Enoxaparin has seen the most ubiquitous use and therefore most people are more comfortable with it compared to dalteparin. There are several advantages to dalteparin: 1) it can be dosed daily, and 2) you may not have to renally dose (though studies on this are limited)7.
Mechanical stuff
Maintain a low threshold to give compression stockings or pneumoboots. There is some risk of skin breakdown, but they are effective.
Diagnosis
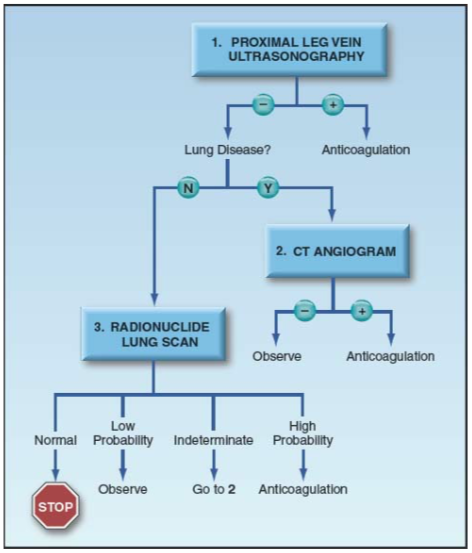
There are no clinical signs that are sensitive and specific for PE. Keep your senses about you when evaluating worrisome patients. D-dimers are probably useless, especially in the ICU setting where every sick patient has an elevated D-dimer. Best to go ahead with lower extremity ultrasounds. The following is a good flowchart for working up a possible pulmonary embolus: