Digoxin
Inotropes are medications that help the heart to operate at higher capacity by increasing the force of ventricular contraction. This causes the Frank-Starling curve to shift upward toward normal, so that at any left ventricular end-diastolic pressure, the cardiac output is greater. Here I describe the actions of digoxin, a previously popular inotrope that has fallen out of favor to other inotropic drugs.
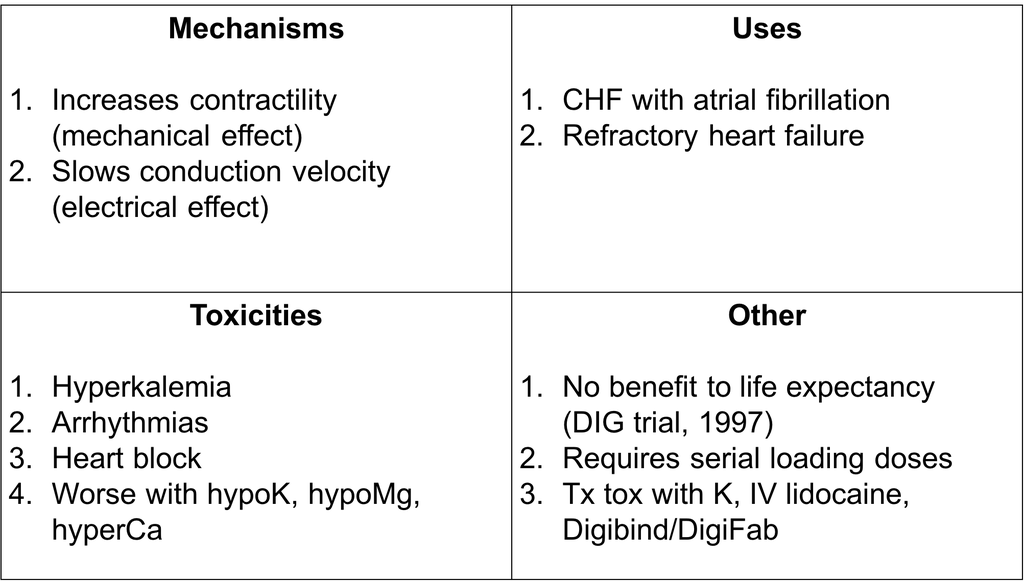
Mechanism
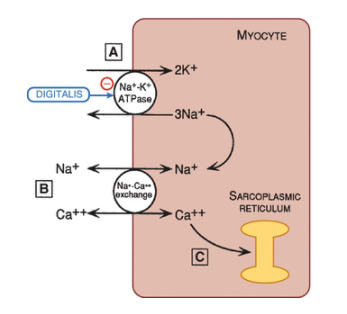
The mechanical effect of digoxin is described below.
- Digoxin inhibits the Na/K ATPase, leading to an increase in intracellular Na+.
- This drives the Na/Ca exchanger, preventing calcium from exiting the cell.
- The increased intracellular calcium gets stored in the sarcoplasmic reticulum.
- When an action potential arrives, an elevated concentration of calcium is released from the sarcoplasmic reticulum and interacts with contractile elements to intensify the force of contraction.
Digoxin also has an electrical effect at the atrioventicular node.
- Digoxin slows conduction velocity at the AV node and increases refractoriness.
- Digoxin also enhances vagal tone and reduces sympathetic activity.
Digoxin can, however, have toxic effects that lead to arrhythmias. It does this through 3 important actions at high doses.
- Less negative resting potential, which slows phase 0 depolarization heterogeneously among conduction cells, enhancing the risk of reentrant arrhythmias.
- Decreased action potential duration, which shortens the refractory period and allows for greater opportunity for propagation of arrhtyhmic impulses.
- Enhanced automaticity, through 1) a less negative resting potential even in nonpacemaker cells, and 2) delayed afterdepolarizations leading to ectopic beats.
Indirect vagal effects can also cause high degrees of AV block.
Uses
When do we use digoxin today?
- CHF complicated by atrial fibrillation (since it also slows the ventricular rate)
- When symptoms do not respond adequately to ACE inhibitors, beta blockers, and diuretics.
Importantly, digoxin does not prolong life expectancy of patients with chronic heart failure.
Pharmacokinetics and toxicity
Digoxin is excreted by the kidneys, and requires loading doses (an initially higher dose of a drug) to achieve therapeutic concentrations. Digoxin may act on the area postrema of the brain to induce nausea. Digoxin can also cause arrhythmias, heart blocks, and tachycardias.
In patients with hypokalemia, hypomagnesemia, and hypercalcemia, digitalis toxicity should be monitored. Administering with amniodarone can also raise serum digoxin concentration through changes in digoxin clearance.
Treatment of digoxin toxicity includes potassium repletion and IV lidocaine for digoxin-triggered arrhythmias. High-grade AV block could be an indication for pacemaker therapy. For severe intoxication, anti-digoxin antibodies may be useful.
Summary